Is there a link between untreated and/or undiagnosed obstructive sleep apnea (OSA)and type 2 diabetes(T2D)?
Untreated OSA may impact your glucose metabolism, promote insulin resistance, and is associated with development of T2D. Obesity is a key contributor to both OSA and the impact of type T2D.
There is a close correlation between sleep apnea and diabetes. Why does that matter? You run a higher risk of T2D and insulin resistance if you have untreated sleep apnea.
Metabolic syndrome
A higher risk of heart disease is associated with this ailment, which includes high blood pressure, abnormal cholesterol levels, excessive blood sugar, and an enlarged waist circumference.
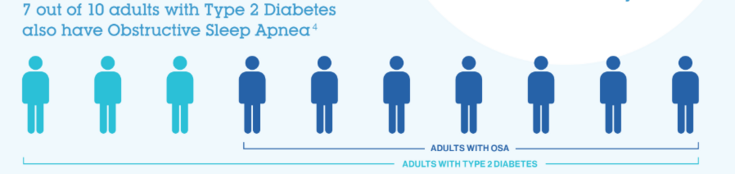
Co-morbidity of OSA and T2D
You are not alone.
Studies have shown:
- There is a range from 20-70 % of patients with Type 2- Diabetes also have concurrent OSA. OSA is associated with an increased risk of developing T2D, independent of other risk factors.
- Treating sleep apnea with a positive airway pressure device may reduce the risks and impacts of T2D.
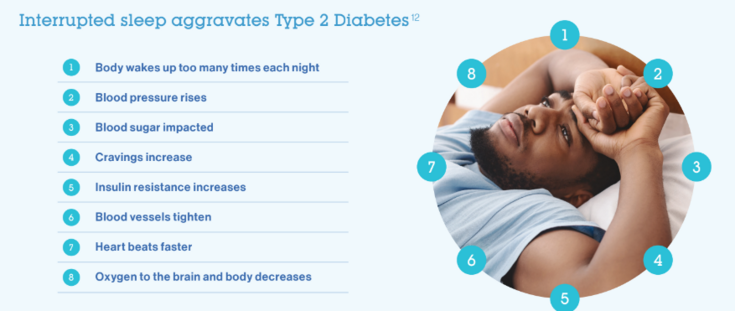
What effect does interrupted sleep have on your Type-2 Diabetes?
Interrupted sleep aggravates Type 2 Diabetes: Body wakes up too many times each night; Blood pressure rises; Blood sugar impacted; Cravings increase; Insulin resistance increases; Blood vessels tighten; Heart beats faster and Oxygen to the brain and body decreases.
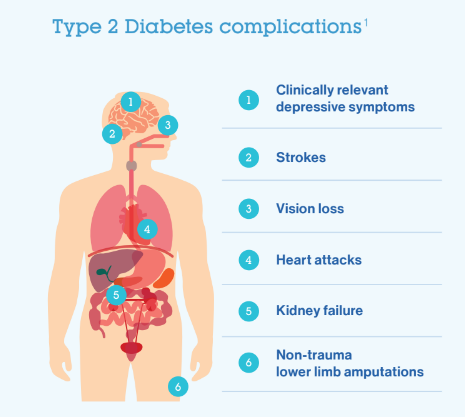
Type 2 Diabetes complications
- Clinically proven depressive symptoms; Stroke; Vision loss; Heart attacks; Kidney failure; Non-trauma lower limb amputations.
Your doctor or healthcare provider has no doubt discussed the complications of untreated or uncontrolled T2D.
OSA can worsen T2D by increasing insulin resistance and impaired glucose metabolism, so it’s important to identify and effectively treat OSA in patients with T2D.
Treating OSA by improving your breathing during sleep, will help negating the effect that interrupted sleep may be having on your ability to control your T2D.
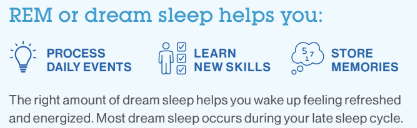
Rapid eye movement (REM) or dreaming sleep:
It is believed that REM sleep is crucial for mood, memories, and learning. The brain is functioning similarly to when we are awake during REM. Lack of REM sleep can have an impact on our mood, memory, and capacity to learn. Your REM sleep may be impacted if you have a sleep disorder, like OSA. The vast majority of dreams occur during the REM sleep stage. Even though sleep apnea can happen at any stage of sleep, it frequently gets worse during REM sleep due to the naturally occurring reduction in muscular tone in the upper airway during REM sleep. In fact, some people only experience apneas and hypopneas during REM sleep. You can dream better if you use continuous positive airway pressure (CPAP) therapy to control sleep apnea.
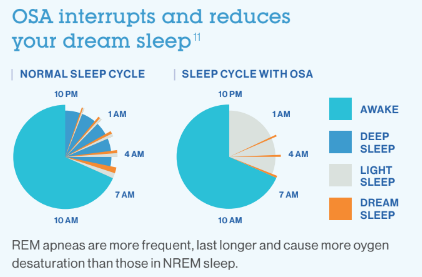
OSA Interrupts and reduces dream sleep:
- Most dream sleep occurs during the latter part of your sleep cycles.
- During a typical night, about 18 to 23% of sleep time is spent in REM sleep. The first period of REM usually lasts around 10 minutes or less, but the amount of time spent in REM sleep usually increases as the night progresses. Later in the night, sleepers may spend around an hour at a time in REM sleep
- During OSA events in REM sleep, the partial or complete obstruction of the upper airway leads to a cessation of airflow and a decrease in oxygen desaturation. The brain senses the decrease in oxygen levels and arouses the individual from sleep to restore airflow. This arousal may only last a few seconds but it disrupts the continuity of sleep and prevents the individual from reaching the restorative deep stages of sleep.
- OSA events during REM sleep are more frequent, last longer and cause more oxygen desaturation than those in the NREM stages
- Treating OSA events during REM sleep is essential for improving sleep quality, reducing daytime sleepiness and improving concentration and cognitive function. OSA events during REM sleep have also be linked to and increased risk of T2D
- This diagram depicts the effect that OSA has on a healthy sleep cycle, you can see the disruptive pattern of OSA on sleep. The nature of sleep loss in OSA is best described as “sleep fragmentation,” whereby deeper stages of sleep are replaced by less restful, lighter stages of sleep.
- Specifically notice the lack of deep sleep and the decreased amount of REM sleep in the OSA patients diagram, robbing patients with untreated OSA of their important dream sleep.
- This highlights the importance of a full night's treatment of your OSA while you sleep. We find that some patients may wake up in the middle of the night, for a number of reasons, and then decide to “treat myself and opt to leave the mask off”. This is not the best option for patients with T2D as it not only robs you of important dream sleep, but studies have shown that OSA events that happen during untreated dream sleep are more severe and can exacerbate your T2D control.
Treating both for a better Quality of Life
Sleep is essential for the proper functioning of all individuals. Sleep-disordered breathing can occur at any age and is a common reason for medical visits, often under-recognized leading to large numbers of undiagnosed people with OSA.
Scientists have discovered a connection between pre-diabetes and sleep disturbance. Sleep apnea has been found to affect diabetes control in many ways. During sleep, in an attempt to regain oxygen through breathing, the body releases stress hormones that can raise blood glucose levels, which, if correct measures are not taken, can lead to diabetes. It is common for those suffering from apnea to eat more often during the . For a few reasons including fatigue and increased hunger which may both occur from sleep fragmentation. In addition, fatigue will result in less motivation to exercise. This combination of higher food intake and less physical activity contributes to the development of diabetes.
“Type 2 diabetes mellitus and obstructive sleep apnea are highly prevalent pathologies that often coexist. There is a high prevalence of sleep apnea in patients with prediabetes and type 2 diabetes mellitus, and vice versa. At the same time, there is an association between sleep apnea and cardiovascular disease.
But what to do? First understand that sleeping badly is not normal!
How do you know if you may have OSA?
If you suspect that you may be suffering from a sleep disorder, seek medical help. The specialist will order tests that monitor your sleep.
The diagnosis can be made by an exam called polysomnography, which is performed sleeping one night in a sleep laboratory or at home (with a level 3 device) , where the patient is monitored by sensors which is performed at home with a level 3 device that records breathing, heart rate, oxygen levels or in a sleep laboratory, level 1 study, which is more comprehensive and measures brain waves and other aspects of sleep that include all night monitoring by a sleep technician.
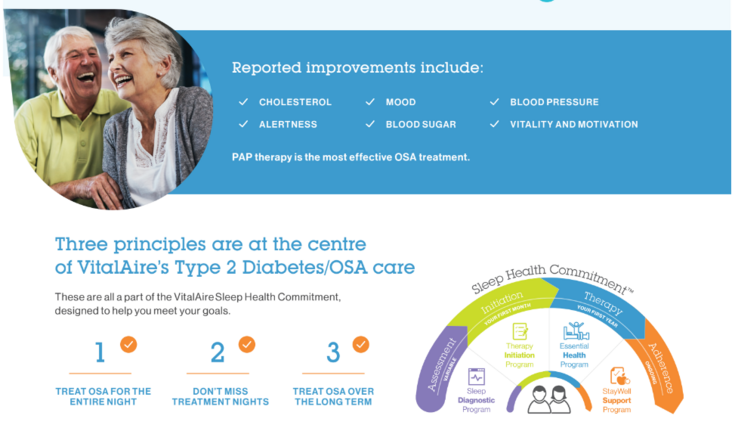
How we can help:
- We are sleep specialists who understand the need for a good night's sleep, that is why we have the Sleep Health Commitment
- Our commitment to you is that we will individualize your care and give you the education and support that you need to get a good night's sleep
- We will work with you on your sleep journey and help to troubleshoot any challenges that you may encounter along the way, so that you can get the sleep that you deserve